- Who can I contact for medical maintenance questions?
- How do I request medical devices that either aren’t on my Modification Table of Organization and Equipment (MTOE) or are above what’s authorized?
- When and how often does a radiation producing medical device require a radiation protection survey?
- What is a Radiation Protection Program File (RPPF)? When and why do I need one?
- What is the approved automated system for tracking medical device maintenance?
- What is the difference between Not Mission Capable (NMC) and an administrative (ADMIN) deadline? Which should I use and when?
- What publications should I be familiar with to perform my job as a 68A/670A in the operating force?
- What is a Global Combat Support System-Army (GCSS-A) Equipment Status Report (ESR) and how is it read and validated?
- How do I know if my medical device is unserviceable and what do I do with an unserviceable device?
- What do I do if my medical device is not on the property book?
- As an operating force Soldier, where do I check for medical device recalls and modifications?
- How do I know if my medical device is ready for patient care?
- How often does a defibrillator need servicing and why?
- What medical-device training resources are available for maintainers?
- Where can I find medical device information or other resources?
- Where can I find a medical device packing/startup list?
- What tools and Test Measurement and Diagnostic Equipment (TMDE) am I authorized?
- What is the Army maintenance standard?
- How do I track maintenance if the Automated Information System (AIS) is down?
- How do I know if my device has an Authority to Operate (ATO) or if I’m allowed to connect a medical device to the network?
- Where do I get support for Test Measurement, and Diagnostic Equipment (TMDE)?
- How often should my Test Measurement, and Diagnostic Equipment (TMDE) be verified?
- How do I determine if my medical device has been serviced or needs maintenance/service?
- As a medical device operator, do I need to perform 10-level maintenance? How can I request maintenance or service for my device?
- What do I need to service the SAVe Ventilator (LIN: V05006, NIIN: 01-581-8155, NIIN: 01-571-1689)
- How do I obtain status on a medical device evacuated to the Medical Maintenance Operations Division (MMOD)?
- What do I need to service the 326 M Suction (LIN: S05058, NIIN: 01-435-0050)?
- What type of air is appropriate for servicing ventilator and anesthesia medical devices?
- How do I pull my on hand and authorization data?
- Why is AR 700-138 (Army Logistics Readiness and Sustainability) important?
- What is a Transaction (T-Code)?
- What should I do to maintain or dispose of medical device batteries?
- What is a PTIL (Publications Tailored Index Listing) and how do I get one?
- What do the markings on a medical oxygen cylinder mean?
- What are Prescribed Load Lists (PLLs) and Shop Stock?
- What equipment is required to service the ZOLL 330 Multifunction Aspirator, LIN: S05058, NIIN: 01-677-5151?
- What items are required to perform services on a Hamilton T-1 Ventilator?
- My commander just asked me to help him write his Commander’s Maintenance Directive. What is the Commander’s maintenance directive and what should it contain?
- How can I find out what tools or Test, Measurement, and Diagnostic Equipment (TMDE) am I authorized?
- How can I get the list of components for the medical equipment maintenance repairman’s and organizational tool boxes?
- What is the Fire Triangle and why is it important when dealing with oxygen systems?
- Who is the only authorized individual that can authenticate a medical device condition code?
- Why is AR 700-4, Logistics Assistance, important for my maintenance activity?
- Can I just replace a broken DEXIS sensor with a new Titanium Sensor?
- What do I do if my medical device harms somebody (patient, employee, etc.) or has a near miss?
- What are the supply condition codes for medical devices?
- What does ALARA mean and what are its basic principles?
- How can I determine if an organization has acknowledged a message in the Modification Management Information System?
- What do the dates found on oxygen and carbon dioxide-sensor packaging mean?
- What is the ECRI Institute and how can I become a member?
- What is medical device lockout/tagout?
- What Preventive Maintenance Checks and Services (PMCS) are required for the Impact (ZOLL) 754M Ventilator?
- As a new maintainer what is one of the best references to find information on field maintenance operations?
- What is the CBET certification and how can I earn it?
- How should the Portable Oxygen Generator System (POGS) feed-air compressor be installed and why is it important?
- What is a maintenance significant medical device?
- What is purpose of the 'Use by' date labeled on the outside of my battery kit?
- What are Scheduled Parts Replacements (SPRs) and how do I manage them?
- What is an Oxygen Compatibility Assessment (OCA)?
- What purpose do Prescribed Load Lists (PLLs) serve? What is shop stock?
Answers
Q: Who can I contact for medical maintenance questions?
A: For immediate assistance contact your next level of medical maintenance support (e.g., Medical Logistics Company or Medical Treatment Facility). If support is not available or can’t be provided, contact Army Medical Logistics Command, Integrated Logistics Support Center, Logistics Assistance Directorate:
usarmy.detrick.amlc.mbx.ilsc-lap@army.mil.
Q: How do I request medical devices that either aren’t on my Modification Table of Organization and Equipment (MTOE) or are above what’s authorized?
A: If additional equipment is needed that exceeds your unit’s authorization or is not authorized, discuss the requirement with your unit’s G-3 (Operations Section) to determine if an Operational Needs Statement (ONS) should be submitted. The ONS is a process used to temporarily document an urgent need for a nonstandard/un-programmed capability to correct a deficiency or improve a capability required for mission accomplishment. ONS submission is a G-3 function written and processed IAW AR 71-9, Warfighting Capabilities Determination (Chapter 6 and Appendix B).
Q: When and how often does a radiation producing medical device require a radiation protection survey?
A: Radiation protection surveys (also referred to as safety compliance/rad surveys) ensure X-ray systems operate according to federal regulations and national standards. The principal goal of a radiation protection survey is to keep patient dose As Low As Reasonably Achievable (ALARA) without reducing the quality of patient care. The concept of ALARA is applied in clinical settings to emphasize the importance of limiting ionizing radiation exposure produced by diagnostic X-ray medical devices. Radiation protection surveys are part of an organization’s Quality Assurance (QA) program for diagnostic X-ray systems improving the benefit-to-risk ratio by optimizing radiation dose and image quality. Radiation protection surveys are performed by (or under supervision of) a qualified expert such as an Army-certified Health Physicist. Under extreme circumstances, exceptions cited in TB MED 521 or stipulated through US Army Public Health Command guidance can be made for locations in other countries or on military vessels.
TB MED 521 requires radiation protection surveys to be performed on radiographic and tomographic X-ray systems before initial clinical use and annually thereafter. If surveys are in a joint-commission accredited facility, they must be performed every two years for intra-oral and panoramic dental radiography equipment or every three years for veterinary radiography systems.
Radiation protection surveys are required after repairs or modifications that may affect patient dose or image quality. Only the affected area of the system must be retested; a resurvey of the entire system is not required. Surveys are additionally not required for system relocation or transport provided no damage has been detected and the system has been tested by a qualified Biomedical Equipment Specialist. If system output has changed or a defect is detected, a new radiation protection survey is required.
Diagnostic X-ray systems in long-term storage don’t require annual surveys. A survey is required, however, when the system is removed from storage and placed into clinical use. The need for X-ray systems deployment availability should be carefully considered before placing the system in long-term storage where the annual survey can lapse.
Survey testing parameters (IAW 21 CFR Chapter 1, Subchapter J) include electrical, mechanical, safety, image quality, and radiation dose as well as shielding/protective equipment and establishment of a performance baseline.
Reference:
- TB MED 521 (2002)
- Federal Guidance Report FGR 14 (2014)
Q: What is a Radiation Protection Program File (RPPF)? When and why do I need one?
A: An RPPF must be maintained for each radiation producing medical device to include initial acceptance documentation, FDA Form 2579, the latest DD Form 2164 (X-ray Verification/Certification Worksheet); the initial (and most current) radiation survey, maintenance history, maintenance work orders, and applicable disposition forms. RPPFs must be established IAW AR 25-400-2 (The Army Record Information Management System) using file number 750-8i. These files are federally mandated under Title 21 CFR, Subchapter J, required under both TB MED 750-2 and 521, and are subject to Command Maintenance Discipline Program (CMDP) inspection.
Q: What is the approved automated system for tracking medical device maintenance?
A: IAW HQDA EXORD 138-21, Global Combat Support System-Army (GCSS-A).
Q: What is the difference between Not Mission Capable (NMC) and an administrative (ADMIN) deadline? Which should I use and when?
A: IAW AR 750-1, NMC is a condition applied to medical devices that cannot perform their health service mission whereas administrative deadline is when equipment is taken out of service by the commander or field-level maintenance officer because they deem it necessary. HQDA EXORD 138-21 states that NMC must be used when medical device scheduled services are not completed. Medical devices should never be administratively deadlined.
Q: What publications should I be familiar with to perform my job as a 68A/670A in the operating force?
A: There are several key publications a 68A/670A can rely on to be successful. TB MED 750-2 (Appendix J) includes a checklist of essential publications and regulations that can be referred to for improving job performance. Common publications used to gain better familiarization include AR 750-1, TB MED 750-2, and local Standard Operating Procedures (SOPs).
Q: What is a Global Combat Support System-Army (GCSS-A) Equipment Status Report (ESR) and how is it read and validated?
A: The ESR documents the status of reportable and non-reportable Not Mission Capable (NMC) medical devices. A good job aid for this is ‘JA Equipment Status Report v4’ found in the End User Manual + (EUM+). To locate this job aid, log into GCSS-A and click the EUM+ link. Access the maintenance button found at the bottom of the screen and click Job Aids in the center of the window; follow instructions to search for the ‘JA Equipment Status Report v4’ job aid. This excellent resource walks through every aspect of the ESR providing examples of real-world scenarios.
Q: How do I know if my medical device is unserviceable and what do I do with an unserviceable device?
A: Only a technically qualified medical maintainer (MOS 68A/670A or Army (1670 Series) Civilian Equipment Specialist) assigned to a maintenance activity can perform a Technical Inspection (TI) for turn in. If a medical device can’t be serviced due to manufacturer discontinuation of repair parts sales or servicing, the medical maintainer will contact the USAMMA, Maintenance Operation Center-Medical (MOC-M) to determine whether repair can be performed by a Medical Maintenance Operations Division (MMOD).
Maintenance is not authorized and the device is deemed uneconomically repairable, when the medical maintainer determines that the estimated cost of repair exceeds the Maintenance Expenditure Limit (MEL) or that the device is no longer manufacturer supported. At this time, the maintainer will assign the device a supply condition code of H indicating that it’s unserviceable (condemned). At the customer’s discretion, a one-time waiver may be requested for device repair IAW AR 750-1. The unit-appointed senior maintenance manager will review, verify, and authenticate condition code assignment by signature endorsement on the maintenance request. This manager will then notify the customer by memorandum and provide a copy of the maintenance historical record and work request. The maintenance request will be closed at this time regardless of the customer’s intent to request a waiver.
The medical device owner is responsible for contacting their Property Book Officer (PBO) for disposition instructions. The PBO will locate disposition instructions entered in the Army Enterprise Portal (AESIP) Lead Materiel Integrator- Decision Support Tool (LMI-DST) by performing the following steps and will provide these instructions to the owner for device turn in:
- Login to the Army Enterprise Portal (AESIP) https://www.aeisip.army.mil/irj/portal dashboard.
- Use Application DST (LMI DST) and select Item Catalog, NIIN/MCN Catalog.
- Search for applicable National Item Identification Number (NIIN) and select NIIN.
- Refer to disposition Instructions in lower window to determine why the device is obsolete, the replacement National Stock Number (NSN), and turn-in instructions.
References:
- USAMMA, MOC-M: 301-619-4378 or usarmy.detrick.usamma.mbx.ops-center@army.mil
- AR 700-142 - Type Classification, Materiel Release, Fielding, and Transfer
- AR 750-1, Chapter 4, Section 4-4 Technical Inspections
- AR 725-50, Table C-38, Supply Condition Codes
- TB MED 750-2, Chapter 7 & 8
- TB MED 7, Chapter 4 & 5
Q: What do I do if my medical device is not on the property book?
A: Ultimately, the device must be collaboratively added with assistance from the Property Book Officer, unit supply representative, unit maintenance manager, and hand receipt holder. Three primary lines of effort are needed to accomplish this task. 1. Identify medical sets and maintainable components. 2. Configure components in systems with parent medical sets (to enable reporting of mission-capability status), and 3. Establish medical device maintenance plans.
References:
- HQDA EXORD 138-21
- Global Combat Support System-Army (GCSS-A) Training Bulletin: TB000647
- GCSS-A Training Bulletin: TB000635
- GCSS-A End User Manual (EUM+)
Q: As an operating force Soldier, where do I check for medical device recalls and modifications?
A: The Modification Management Information System (MMIS) has a Class VIII module allowing units owning medical devices to receive, track, and respond to Medical Materiel Quality Control (MMQC) messages for medical device recalls and alert messages. IAW AR 40-61, MMIS enables users at all levels to determine the safety status of their equipment down to the serial-number level. Search options include: messages that have been applied/completed (compliant), messages that remain to be applied/completed (non-compliant); copies of MMQC messages in the MMIS library, the coordinator’s directory, training links, and a user’s manual. To access MMIS, login to
https://www.logsa.army.mil and navigate to the Logistics Information Warehouse (LIW) tab located at the top of the page; new LOGSA users must register to obtain LIW access. Basic read-only MMIS access is granted automatically to all LIW users.
Q: How do I know if my medical device is ready for patient care?
A: IAW TB MED 750-2, check the equipment record in Global Combat Support System-Army (GCSS-A) or ask your medical maintenance section.
Q: How often does a defibrillator need servicing and why?
A: Defibrillators should be calibrated according to manufacturer specifications or at lease semiannually. IAW AR 750-1 as well as international, federal, and state law, a safe environment must be provided to prevent electrical shock and other safety hazards related to medical equipment use.
Reference:
- AR 750-1
- TB MED 750-2
- Title 21 CFR Section 1020, Subchapter J
- NFPA/ANSI
- Manufacturer literature
- AR 40-61
Q: What medical-device training resources are available for maintainers?
A: Deployable online (web-based) medical device training courses are available from the M2PA Knowledge Management Center (KMC) located at
https://www.milsuite.mil/book/docs/DOC-598431.
Those with access to ECRI Institute services can take advantage of many health-technology resources such as webinars, online learning modules, and personalized education/training services; for information, visit
https://www.ecri.org/. A variety of online and resident courses are typically offered by manufacturers; for information on course availability, contact manufacturers directly.
Reference:
- M2PA KMC milBook
- ECRI Institute
- Manufacturer
Q: Where can I find medical device information or other resources?
A: Visit the AMLC Medical Materiel Information Portal (MMIP) at
https://a01.usamma.amedd.army.mil/mmip/Secure , request assistance through the Policies & Analysis (P&A) Directorate milBook Knowledge Management Center (KMC) located at
https://www.milsuite.mil/book/groups/m2pa, or contact the medical device manufacturer.
Reference:
- AMLC MMIP
- P&A Directorate KMC milBook
- Manufacturer
Q: Where can I find a medical device packing/startup list?
A: Visit the Medical Materiel Information Portal (MMIP) at
https://a01.usamma.amedd.army.mil/mmip/Secure.
Reference:
Q: What tools and Test Measurement and Diagnostic Equipment (TMDE) am I authorized?
A: TMDE authorizations are available from the US Army Directorate of Force Management. Visit FMSWeb at
https://fmsweb.fms.army.mil/unprotected/splash/. Additional information is available from the Global Combat Support System-Army (GCSS-A) BI Launch Pad under the property book file. A link can be obtained from End User Manual + (EUM+).
Q: What is the Army maintenance standard?
A: The 10-level standard is a medical device with all accessories needed to perform its basic functions. The 20-level standard is a medical device that has an updated medical-maintenance service completion. AR 750-1 refers to the Army 10/20 standard as one maintenance standard defined by the TM 10/20 series or appropriate/applied technical data plans. Army medical devices meet the 10/20 standard when:
- Fully Mission Capable (FMC)
- All faults are identified IAW prescribed intervals using the ‘items to be checked’ column of applicable TM 10/20 series Preventive Maintenance Checks and Services (PMCS) tables.
- Required parts and supplies are available to perform all repairs, services, and related work that correct field-level medical devices or materiel faults for completion in accordance with DA PAMs 738-751 and 750-8.
- Parts and supplies are required to complete corrective actions but are not available in the unit and are on a valid funded requisition in accordance with AR 710-2.
- Corrective actions (not authorized at field level by applicable Technical Manual (TM) or Maintenance Allocation Chart) require evacuation to the next higher level of support (sustainment) and use appropriate turn-in documentation as cited in AR 710-2 and DA PAM 710-2-1 for turn-in to supply.
- Scheduled services are performed IAW the required (technical publication) service interval. Due to competing mission requirements, units are authorized a 10-percent variance when performing scheduled services IAW DA PAM 750-8 for ground equipment and TM 1-1500-328-23 for aviation equipment. Afloat pre-positioning ships are excluded from this variance requirement.
- All routine, urgent, and emergency maintenance work orders are applied to medical devices and reported in the Modification Management Information System (MMIS) IAW AR 750-10.
- All authorized BII and COEI are present and serviceable on a valid supply request.
Q: How do I track maintenance if the Automated Information System (AIS) is down?
A: Manual forms are used to record maintenance services. TB MED 750-2 calls for the use of DA Form 2404 (Equipment Inspection and Maintenance Worksheet) or DA Form 2407 (Maintenance Request) to manually track scheduled and unscheduled work-item maintenance services IAW DA PAM 750-8, TB 38-750-2, and local procedures. Manual maintenance tracking is performed when there are inadequate automated maintenance procedures. Maintenance activities must retain a copy of all manual maintenance-request forms for a period of one year following the close date.
Q: How do I know if my device has an Authority to Operate (ATO) or if I’m allowed to connect a medical device to the network?
A: Before connecting a medical device to the network, contact your unit's S6/G6 shops as well as the medical device Materiel Developer (MATDEV) located at the US Army Medical Materiel Development Activity (
https://www.usammda.army.mil/index.cfm/about/contact_us) for applicable guidance.
Reference:
- Local S6/G6 SOP
- AMLC Website
Q: Where do I get support for Test Measurement, and Diagnostic Equipment (TMDE)?
A: The local (or closest) TMDE Support Activity (TSA) schedules and manages verification/calibration services for all general and special purpose TMDE (TMDE-GP and TMDE-SP). The Army’s TMDE program is administered by the US Army TMDE Activity (USATA). TMDE-GP is fully supported by the USATA, is authorized at many activities, and used for the diagnosis/repair of medical devices. TMDE-SP is used for specialized applications such as medical device verification and calibration services. Special support, however, may be required to service TMDE-SP through the Original Equipment Manufacturer (OEM), Medical Maintenance Operations Division (MMOD) Tracy, CA., or through US Army Medical Materiel Center-Europe (USAMMC-E). IAW TB 43-180, para 6-l, owning units are responsible for coordinating medical TMDE-SP shipments destined for the MMOD Tracy calibration facility. In addition, the owning unit is responsible for notifying the supporting unit of the new calibration due date upon return of TMDE. All medical maintenance support organizations with general or special purpose TMDE requiring calibration services must register this TMDE with the local (or closest) TSA. IAW AR 750-43, each command, installation, or unit that uses general or special purpose TMDE will designate a TMDE Calibration and Repair Support (C&RS) coordinator in writing. This coordinator serves as a central Point of Contact (POC) for all TMDE C&RS matters. TB 43-180 specifies the responsible TMDE calibration support facility; when calibration cannot be performed by this facility, contact the local (or closest) TSA for assistance. TMDE-GP may be performance-verified and calibrated by the:
- Local (or closest) TSA
- Army Maintenance Support Company (AMSC)
- Area TMDE Support Team (ATST)
- TMDE Support Center (TSC)
To avoid servicing conflicts, keep track of time when TMDE goes in for service. Request status from your local (or closest) TSA or from MMOD Tracy. Contact information for MMOD Tracy can be found in SB 8-75-S6. If your TMDE won’t make it back in time to perform equipment services, attempt to borrow TMDE from local medical maintenance activities (i.e., other Brigade Combat Teams, combat support hospitals, hospital centers, medical logistics companies, or local Medical Treatment Facility (MTF)). As a last resort, request loaner TMDE from MMOD Tracy through your command. If possible, always try to schedule TMDE service support during periods when the medical device it supports is off cycle for scheduled services.
References:
Q: How often should my Test Measurement, and Diagnostic Equipment (TMDE) be verified?
A: TMDE calibration intervals are initially designated by the Materiel Developer (MATDEV)/Program Manager (PM) when it first enters Army inventory. When TMDE is fielded to the unit, all required maintenance information is provided. If it isn’t, the Biomedical Equipment Specialist (BES) must request this information from the fielding team. IAW AR 750-43, users in receipt of TMDE must coordinate with the supporting TMDE Support Activity (TSA) to enter the device into the TMDE Integrated Materiel Management System (TIMMS). The calibration/verification schedule is included with device information in TIMMS. The TSA notifies the user when TMDE is approaching its services due date; it’s the user’s responsibility to ensure device availability. Following initial calibration/verification (and to prevent established schedule/equipment record conflicts) an item will normally be scheduled and calibrated based on the interval specified at the time of the last calibration. Calibration/verification information can also be found in TB 43-180.
Q: How do I determine if my medical device has been serviced or needs maintenance/service?
A: IAW TB MED 750-2, determine if your medical device has been serviced by checking the equipment record in Global Combat Support System-Army (GCSS-A) or ask your medical maintenance section. Preventive, Maintenance, Checks and Services (PMCS) is required prior to device use, to determine if planned maintenance is required, use the ZMPRPT Technical Code (T-Code) in GCSS-Army or ask your supporting medical maintenance activity. The medical device operator can also ask their supporting medical maintenance activity which will perform required maintenance or service.
References:
Q: As a medical device operator, do I need to perform 10-level maintenance? How can I request maintenance or service for my device?
A: 10-level maintenance is important. Operators are the first line of support for medical device sustainment and have direct responsibility for its daily care. Operators should refer to manufacturer literature as their primary resource for service guidance. If a Preventive Maintenance Checks and Services 10 (PMCS10) is available, the operator should use it to determine required service tasks and for supporting guidance pertaining to a medical device in a Not Mission Capable (NMC) status. AR 40-61 calls for medical device operators to:
- Perform PMCS before, during, and after operation IAW manufacturer literature or the applicable Technical Manual (TM).
- Change user-replaceable components and accessories.
- Use TMs, manufacturer literature, and local Standard Operating Procedures (SOPs) for operator-maintenance guidance.
- Request appropriate maintenance-organization support for repairs/services beyond the scope of operator maintenance.
To request device maintenance or service, check with your supervisor to see if your organization has a Biomedical Equipment Specialist (BES) and ask if the BES published an external Standard Operating Procedure (SOP). If so, consult the SOP and follow published the instructions. If an SOP is not available, contact the BES for guidance on how to submit a medical device work order and ask for a copy of the SOP at that time. If your organization doesn’t have a BES, ask your supervisor who the medical maintenance support activity is and whether they published an SOP. If your supervisor doesn’t know, your command staff will; continue following your chain of command until maintenance support is found. Regardless of who your medical device support provider is, a work order must be initiated describing the equipment (National Stock Number (NSN), serial number, nomenclature, and problem). Provide the work order and associated medical device to the medical maintenance support activity.
References:
- AR 40-61 Medical Logistics Policies
Q: What do I need to service the SAVe Ventilator (LIN: V05006, NIIN: 01-581-8155, NIIN: 01-571-1689)?
A: The following list is what you need to service the SAVe Ventilator (LIN: V05006, NIIN: 01-581-8155, NIIN: 01-571-1689):
- SAVe Preventive Maintenance Manual (Rev. A)
- Inspection Form - SAVe kit (Pages 25-26 of Preventive Maintenance Manual)
- Calibration Form (Page 27 of Preventive Maintenance Manual)
- Test SAVe Patient Circuit
- Michigan Instruments 3600i Test Lung
- Pneuview Software
- Computer capable of running Pneuview software and connecting to Michigan Instruments 3600i Test Lung
- Safety Analyzer
References:
- SAVe Preventive Maintenance Manual (Rev. A)
Q: How do I obtain status on a medical device evacuated to the Medical Maintenance Operations Division (MMOD)?
A: MMODs don’t input work order information into Global Combat Support System-Army (GCSS-A). Customers requesting status must contact the US Army Medical Materiel Agency, Medical Maintenance Management Directorate (M3D), Maintenance Operation Center-Medical (MOC-M) at 301-619-4378 or
usarmy.detrick.usamma.mbx.ops-center@army.mil to obtain medical device status. When requesting status, medical device serial number, the sending Unit Identification Code (UIC), and owning UIC if different than the sending UIC must be provided.
Q: What do I need to service the 326 M Suction (LIN: S05058, NIIN: 01-435-0050)?
A: The following list is what you need to service the 326 M Suction (LIN: S05058, NIIN: 01-435-0050):
- 326 M Suction Unit Operation and Service Manual (Rev. T, 02/09)
- Oscilloscope, DC, Triggered, with a minimum 5-second horizontal sweep, storage capability desirable.
- Small slotted screwdriver
- Stopwatch, minimum 0.1 second resolution
- Regulated DC-Power Supply (5-Ampere minimum rated output)
- Vacuum Gauge
- Safety Analyzer
References:
- 326 M Suction Unit Operation and Service Manual (Rev. T, 02/09)
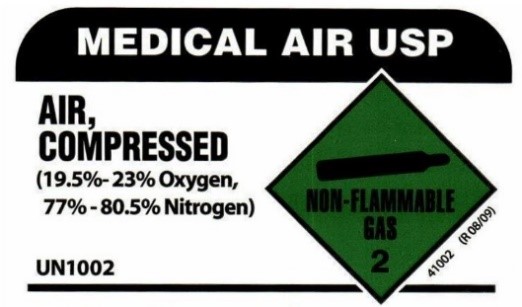
Q: What type of air is appropriate for servicing ventilator and anesthesia medical devices?
A: Medical-grade air. Medical air is a clean, dry gas mix comprised of 19.5-to-23.5-percent oxygen and 77-to-80.5-percent nitrogen. Gas delivery can be supplied by cylinder or medical air compressor. When using compressed cylinders ensure that they are properly labelled: Air, Compressed (Medical Air US Pharmacopoeia (USP)). Note the differing color conventions applicable to International Organization for Standardization (ISO) and US medical-air cylinder labeling, as illustrated below. When using a medical air compressor, ensure that it is properly designated as producing medical-grade air.

References:
Q: How do I pull my on hand and authorization data?
A: Global Combat Support System-Army (GCSS-A) uses the Technical Code (T-Code) ZMATCOM to display materiel pertaining to the property book (on hand) as well as materiel authorizations.
Reference:
- End User Manual + (EUM+) - Run the Mat Comp Report (ZMATCOMP)_001.pdf
- Property Book Officer (PBO)
Q: Why is AR 700-138 (Army Logistics Readiness and Sustainability) important?
A: AR 700-138 prescribes policy and provides procedures for collecting and reporting the physical condition of Army medical materiel. This regulation outlines the reporting responsibilities and requirements of Direct Reporting Unit (DRU) commanders when reporting the readiness status of their medical devices. It additionally outlines medical device readiness goals, methods for submitting equipment readiness status, and frames what medical devices are reportable and how these devices are to be reported (i.e.) Fully Mission Capable (FMC) and Not Mission Capable (NMC)).
Reference(s): AR 700-138
Q: What is a Transaction (T-Code)?
A: The T-code is a short cut (code or key) used to a view the data output screen In Global Combat Support System-Army (GCSS-A) and all SAP-type databases. Instead of using the SAP easy-access menu, the T-Code can be entered into a standard toolbar command field for navigation to a specific screen. Many available T-Codes are written to industry standard. T-Code's beginning with the letter Z are custom codes created for the end user (e.g., ZMPRPT (Maintenance Plan Report Front End) in GCSS-A). T-codes are designed to represent data in a usable/searchable format and are limited by roles and responsibilities assigned to the user.
Reference(s): GCSS-ARMY SMART BOOK (Release 3.0) pg4 1,
https://www.saphub.com/abap-tutorial/what-is-sap-transaction-code/2
Q: What should I do to maintain or dispose of medical device batteries?
A: Follow manufacturer recommendations for use, storage, and disposal of batteries to prolong battery life and ensure safe medical device operation. Here are some tips:
Battery use - Batteries operate and charge over wide temperature ranges but there are limits to battery charging and the use of batteries in extreme (high/low) temperature conditions.
Battery storage - Depending chemistry type, rechargeable batteries should be stored in a charged condition. Some batteries need to be recharged every few months during storage while others just need a recharge before use. Remove alkaline batteries from medical devices before placing your device in long-term storage.
Battery Disposal - Do not place used batteries in the trash. Understand and follow installation/unit guidance for battery disposal. If battery disposal policies don’t exist, work with your unit’s safety officer to develop a policy in compliance with applicable local and regulatory guidance. Proper battery disposal will protect the environment from harmful chemicals.
Always consult manufacturer literature for specific guidance on battery powered medical devices in your inventory.
Reference(s):
Q: What is a PTIL (Publications Tailored Index Listing) and how do I get one?
A: The PTIL is a record of all Army Materiel Command (AMC) equipment publications for an individual unit, often determined by the unit’s Unit Identification Code (UIC). To request a PTIL, send an email to
usarmy.redstone.logsa.mbx.eopdb@mail.mil and provide the following:
- Information:
- UIC(s)
- Detachments only: send LINs (single column excel)
- Maintenance levels
- Name, phone, military address
- Reports reflecting ‘AUTHORIZED’ equipment from Modified Table of Organization Equipment (MTOE) and on-hand but not authorized from property book.
- PTIL recommended for:
- Change of Command
- Prior Development
- At Deployment
- Redeployment
- Annually
For PTIL related help or questions anyone can phone: (256) 955-8586 (DSN: 645-8586) or (256) 313-6115 (DSN: 897-6115).
Reference:The Logistics Data Analysis Center (LDAC) website at:
https://www.logsa.army.mil/#/
BACK TO TOP
Q: What do the markings on a medical oxygen cylinder mean?
A: Oxygen cylinders are marked to designate the type of cylinder, maximum fill pressure, hydrostatic test date, inspector, manufacturer, and serial number. Markings are normally stamped into the shoulder of the cylinder. The hydrostatic test date and inspector mark indicate when the cylinder was last tested and who tested the cylinder. Most oxygen cylinders are required to be tested every 5 years. Hydrostatic testing ensures that the cylinder can safety hold its maximum fill pressure. There are two other markings that are sometimes found on these cylinders. The plus (+) sign located after the test date designates that the cylinder can be filled to 10% above the pressure stamped on the cylinder. The five-pointed star in the same location designates that the hydrostatic test date has been extended an additional 5 years. A cylinder with a five-pointed star would need to be tested every 10 years.
References:
- 49 CFR 178.3 - Code of Federal Regulations, Title 49 Transportation, Department of Transportation (DOT), Part 178.3 Marking of Packaging.
- 49 CFR 180.213 – Code of Federal Regulations, Title 49 Transportation, DOT, Part 180.213 Requalification Markings.
BACK TO TOP
Q: What are Prescribed Load Lists (PLLs) and Shop Stock?
A: PLLs are maintenance repair parts that are demand supported, non-demand supported, or are new repair parts for new end items. These repair parts are kept to support a unit’s daily maintenance program. Demand-supported unit maintenance repair parts are parts that have been ordered six or more times within a control period to qualify for initial stockage. Major Army commands may authorize a 180-day or 360-day control period.
Shop stock represents demand-supported repair parts and consumables stocked within an authorized support-level maintenance activity. They are used to accomplish maintenance requests or to facilitate scheduled supported-unit repairs. Shop stock is similar in purpose to repair parts and is kept by a unit in support of organizational maintenance. Shop-stock parts are for internal use only and are issued from an Authorized Stockage List (ASL) at a Supply Support Activity (SSA).
Reference: AR 710-2, Inventory Management Supply Policy below the Wholesale Level; 2-21 and 2-23
Q: What equipment is required to service the ZOLL 330 Multifunction Aspirator, LIN: S05058, NIIN: 01-677-5151?
A: The following equipment is required to perform scheduled services on the ZOLL 330 Multifunction Aspirator.
- 330 PM Test Kit (REF: 8600-000020-01); the following are included in the kit:
- Jar, disposable with Lid (REF: 410-0004-00)
- Kit, Hose, M330 (REF: 540-0050-00)
- Brass Barbed Hose Fitting 3/8” Hose ID, 1/3 NPTF (Female End) (REF: 0301-000344)
- Straight One-Way Valve (Check Valve) 22M to 22F (REF: 0301-000070)
- An extra, fully charged, 330 Multifunction Aspirator battery
- ZOLL 330 Multifunction Aspirator Maintenance Tests Checklist: Found in Appendix A of Service Manual
*Below image is of the Aspirator properly setup for calibration verification*

Reference(s): ZOLL 330 Multifunction Aspirator Service Manual (9650-000278-01 Rev. 1)
Q: What items are required to perform services on a Hamilton T-1 Ventilator?
A: Service of the Hamilton T-1 (LIN V99788, NSN 6515-01-648-5814) requires an assortment of maintenance resources including maintenance consumables, standard tools, Test, Measurement and Diagnostic Equipment (TMDE) connectors, tubing, and adaptors, and service software.
The following sections and pages from the service manual list the required Hamilton T-1 maintenance items:
1. Preventive Maintenance Consumables - Service Manual Section 7.1.2, Page 83.
2. Standard Tools - Service Manual Section 12.2, Page 315.
3. Test Measurement and Diagnostic Equipment - Section 12.3, Page 316.
4. Connectors, tubing, and adapters - Section 12.4, Page 318.
5. Service Software - Section 9, Page 94.
Reference(s): Hamilton T-1 Service Manual, 624393.03, 2.2.x, 27 September 2016.
Q: My commander just asked me to help him write his Commander’s Maintenance Directive. What is the Commander’s maintenance directive and what should it contain?
A: The Commanders Maintenance Directive establishes basic maintenance policies and responsibilities for the performance of the activity’s medical device maintenance mission. In accordance with TB MED 750-2, paragraph 1-6.a, commanders with an organic medical device repair capability (68A, Biomedical Equipment Specialist) will publish a unit level maintenance policy or Commanders Maintenance Directive. It is the BES responsibility as the medical device subject matter expert to assist the commander in this endeavor. The commander’s maintenance directive should at least include the following items:
- Establish the requirement for performance and tracking of operator medical device maintenance.
- Establish the program for the performance of scheduled and unscheduled services.
- Require that any maintenance significant item classified as a medical device or any maintenance significant component are maintained by the medical maintenance activity.
- Identify the individual(s) having authority to approve waivers of maintenance expenditure limits (MEL), and procedures for processing a request for a waiver.
- Define the commander's policy for handling items that cannot be located for the performance of scheduled maintenance services.
- Identify the point of contact for reporting incidents under the Safe Medical Device Act of 1990.
- Establish BES proficiency and sustainment training program.
There is a sample Commander’s Maintenance Directive on page 80 of TB MED 750-2, dated November 2006.
Reference(s): TB MED 750-2, Operating Guide for MTOE Medical Equipment Maintenance, November 2016
Q: How can I find out what tools or Test, Measurement, and Diagnostic Equipment (TMDE) am I authorized?
A: TMDE authorizations can be found in the US Army Directorate of Force Management, Force Management System Website (FMSWeb):
https://fmsweb.fms.army.mil/unprotected/splash/. After logging in, you can identify a unit’s authorizations by looking up the unit’s Table of Distribution and Allowances (TDA) or Modified Table of Organization and Equipment (MTOE). TDA and MTOE searches can be done by searching using the organization name, UIC, document number, location, or more. Once located you can view the TDA or MTOE authorized equipment by clicking on “Equipment Details.”
Reference: US Army Directorate of Force Management, Force Management System Website (FMSWeb)
Q: How can I get the list of components for the medical equipment maintenance repairman’s and organizational tool boxes?
A: If your organization has a publications account you can order the supply catalogs SC 5180-8-A11 and SC 5180-8-A14 at the Army Publications Directorate (APD) website located at URL:
https://armypubs.army.mil/ProductMaps/PubForm/SC.aspx. If you do not have access to a publications account you can get tool case content lists on the Medical Materiel Information Portal (MMIP) URL:
https://a01.usamma.amedd.army.mil/mmip/Secure for Tool Kit Medical Equipment Maintenance and Repair: Org. Maint, NSN: 6545-01-662-0036 at URL:
https://a01.usamma.amedd.army.mil/mmip/Content/filestore/Handbooks/UA8009_Tool%20Kit%20Medical%20Equipment%20Maintenance%20and%20Repair%20Biomedical%20Unit_110717.pdf and Tool Kit Medical Equipment Maintenance and Repair: Repairmans, NSN: 6545-01-659-4025 at URL:
https://a01.usamma.amedd.army.mil/mmip/Content/filestore/Handbooks/UA8008_Repair%20Set,%20Biomedical%20Equipment%20Specialist%20Unit%20Assemblage_110717.pdf and NSN: 5180-00-611-7923, https://a01.usamma.amedd.army.mil/mmip/Content/filestore/Start-Ups/5180-00-611-7923_TOOL%20KIT%20MEDICAL%20EQUIPMENT%20MAINTENANCE_HANDBOOK_INSERT_STARTUP_011918.pdf.
References: Army Publications Directorate (APD) website located at URL:
https://armypubs.army.mil/ProductMaps/PubForm/SC.aspx and Medical Materiel Information Portal (MMIP) URL:
https://a01.usamma.amedd.army.mil/mmip/Secure
Q: What is the Fire Triangle and why is it important when dealing with oxygen systems?
A: The Fire Triangle is used to represent the three elements required to support combustion or fire. It is made up of oxygen, fuel, and an ignition source. If any leg of the triangle can be eliminated or controlled, fire risk can be greatly reduced.
Oxygen pressure and concentration have significant effects on the flammability and ignitability of materials. In general, materials are easier to ignite and burn more readily as oxygen pressure or concentration increase. Ignition risk rises at concentrations as low as 24 percent and pressures as low as 50 pounds per square inch. It is also impossible to eliminate the oxygen leg of the triangle especially when dealing with oxygen systems.
Fuel is any material that can be ignited and burned. Some materials are more difficult to ignite than others. Additionally, some materials when ignited are more resistant to sustained burning than others. Materials also vary in the amount of energy they release when they burn. Materials not normally thought of as fuel in 21 percent oxygen burn readily in high concentrations. Materials such as aluminum, which would normally not burn in ambient air, will burn readily in high concentrations of oxygen. Fuel is another leg of the triangle that is impossible to eliminate.
Commonly recognizable ignition mechanisms include heat, sparks, and friction. Due to the nature of oxygen systems, other less recognizable ignition mechanisms include particle impact, rapid pressurization, flow friction, and resonance. The key to the reduction of oxygen fire risk is the control of ignition mechanisms. This is done through proper selection of materials, system design, cleanliness, safe operating practices, and proper maintenance. Understanding and controlling ignition mechanisms is the key to safe operation and maintenance of oxygen systems.
References: Guide for Oxygen Compatibility Assessments on Oxygen Components and Systems, NASA/TM-2007-213740, March 2007.
Q. Who is the only authorized individual that can authenticate a medical device condition code?
A. The Senior maintenance manager assigned to the unit will review, verify and authenticate condition codes assigned with a signature endorsement on the work order. The senior maintenance manager, medical maintenance Officer in Charge (OIC) or Non-Commissioned Officer in Charge (NCOIC), if an OIC is not assigned, must sign all work orders for condition coded medical devices.
Reference(s): TB MED 750-2
Q: Why is AR 700-4, Logistics Assistance, important for my maintenance activity?
A: AR 700-4 establishes policies and procedures for the Logistics Assistance Program (LAP). The LAP is a program that is meant to provide technical resources to assist unit commanders in identifying and resolving materiel and logistics systems problems that are beyond the capability or responsibility of the using field command. The LAP provides technical resources from each life-cycle logistics command (LCMC) in the form of logistics assistance representatives (LARs). LARs are subject matter experts assigned to Army Field Support Brigades, Battalions, and logistics support teams. Maintenance activities and commanders requiring assistance can leverage the LARs to receive technical advice, training, and coordinating assistance from their respective LCMCs.
Reference(s): AR 700-4, Logistics Assistance
Q: Can I just replace a broken DEXIS sensor with a new Titanium Sensor?
A: While replacing the sensor is the only physical exchange of hardware that will ever be completed on the DEXIS system, it is more involved than that. It requires a current version of the DEXIS software and sensor drivers. The Titanium Sensor will only work with DEXIS software version 9.4.8 or later (version 9.5.0 is recommended). This software can only be downloaded from the DEXIS website at the below link, it is not sold or shipped separately. Therefore, keeping the DEXIS software current while in garrison will prove invaluable if you need to replace the sensor while deployed.
Dexis Software, Version 9.5.0:
https://embed.widencdn.net/download/kavokerr/wrh8fskbh1/DEXIS_950b3_International.zip?u=a0aubk
The Titanium sensor is shipped with a thumb drive containing the Kavo Intra Oral Sensor Drivers which need to be installed unless the previous sensor was also a Titanium. Updated versions of the drivers can be downloaded at the following link.
Titanium Sensor Drivers:
https://embed.widencdn.net/download/kavokerr/aqgongztin/KaVo_IOsensor_Driver_1.0.9.2.zip?u=a0aubk
NOTE: DEXIS system laptops require updating to Windows 10 to meet current Army standards.
For more information about updating your Dental Filmless Imaging System please contact:
US Army Medical Materiel Development Activity Warfighter Deployed Medical Systems PMO Contact Contact Info: (301) 619-3949, usarmy.detrick.medcom-usamma.mbx.crm@mail.mil
Reference: DEXIS Titanium Sensor User Manual, 1.013.1455 REV B, 1 August 2018
Q: What do I do if my medical device harms somebody (patient, employee, etc.) or has a near miss?
A: The answer to this question lies in several different regulatory publications at the federal and Army levels the Federal Food, Drug and Cosmetic Act (FD&C Act) of 1938, the Safe Medical Devices Act (SMDA) of 1990 which amended the FD&C Act, AR 750-1 and TB MED 750-2. The FD&C Act and SMDA are established in Title 21 Chapter 9 of the United States Code.
The Medical Device Reporting (MDR) regulation, section 519(a) of the FD&C Act as amended by the SMDA of 1990, requires medical device users to submit a report whenever they believe that a medical device has caused or contributed to a death, illness, or injury.
AR 750-1, page 118, para 8-10.a., requires all Army organizations to submit a product quality deficiency report (QDR) to report below-standard quality, workmanship or materiel deficiencies of Army equipment.
TB MED 750-2, page 6, para 2-6, requires Biomedical Equipment Specialists to report medical devices determined to be harmful or defective to the extent that its use has caused or may cause serious injury, serious illness, and/or death to either a patient or equipment operator. Do this by submitting a medical materiel complaint (QDR) on a Standard Form (SF) 368. Reporting instructions for Product QDRs are contained in AR 702–7–1, DA Pam 738–751, and DA Pam 750–8.
Reference(s): Title 21 Chapter 9 of the United States Code; FD&C Act of 1938; SMDA of 1990; AR 750-1; TB MED 750-2.
Q: What are the supply condition codes for medical devices?
A: IAW TB MED 750-2, 8-8, supply condition codes are used to classify the operational state of medical materiel. These codes specifically identify the degree of serviceability, condition, and readiness for issue/use. Condition codes also identify actions underway to change the status of materiel. Medical maintenance activities are responsible for assigning medical-device supply condition codes as warranted, including:
- A - Serviceable medical devices with more than six months of life expectancy remaining.
- B - Serviceable medical devices with less than a six-month life expectancy remaining or medical devices that have reached/exceeded life expectancy.
- F - Unserviceable, economically reparable medical devices.
- H - Unserviceable, uneconomically reparable medical devices that do not meet the criteria to justify repair (e.g., exceeding the Maintenance Expenditure Limit (MEL)). Devices for which repair parts are no longer available qualify for H code condition code assignment. Check with the USAMMA cannibalization point located at Medical Maintenance Operations Division (MMOD) Hill, UT to determine alternative parts availability.
Reference(s): TB MED 750-2, Operating Guide for MTOE Medical Equipment Maintenance
Q: What does ALARA mean and what are its basic principles?
A: Ionizing radiation, emitted from radiography equipment, can cause dangerous changes to human tissue including risk of genetic mutations and cancer. These changes are irreversible and cumulative over a lifetime. It is therefore essential that maintainers understand the meaning and practice the principles of ALARA.
As defined in 10 CFR 20, ALARA (as low as is reasonably achievable) means making every reasonable effort to maintain exposures to radiation as far below the dose limits as is practical consistent with the purpose for which the licensed activity is undertaken, taking into account the state of technology, the economics of improvements in relation to state of technology, the economics of improvements in relation to benefits to the public health and safety, and other societal and socioeconomic considerations.
To maintain dose “As Low As Reasonably Achievable”, maintainers should follow these three safety principles:
- Time: Minimize the time of exposure.
- Distance: Double the distance between your body and the radiation source; this reduces the radiation exposure by a factor of four.
- Shielding: Use absorber materials such as Plexiglas® for beta particles and lead for X-rays and gamma rays.
References: Code of Federal Regulation 10 CFR 20.1003, Standards for Protection Against Radiation.
Q: How can I determine if an organization has acknowledged a message in the Modification Management Information System?
A: MMIS provides a command-level confirmation rollup delivering a snapshot status view for all confirmation requirements. This report summarizes quantity required, confirmed, and not confirmed and additionally permits drilldown into a single category via hyperlink. To identify who has or has not confirmed message receipt, a user must perform the following steps: 1) Login to MMIS. 2) Select ‘Confirmation Rollup’ under the appropriate section (i.e., safety message section, Class VIII Messages section, etc.). 3) Select an available message or search using the message number. 4) Display details by clicking one of the hyperlinked quantities under the associated command.
Reference: MMIS HelpDocument:
https://liw.logsa.army.mil/mmis/api/help/help Document.pdf
Q: What do the dates found on oxygen and carbon dioxide-sensor packaging mean?
A: Oxygen and carbon dioxide sensor packaging may display a date of manufacture or Use by. If dated, one of the two symbols illustrated below should be displayed adjacent to the date stamp denoting its meaning. These symbols originate from International Organization for Standardization (ISO) 15223-1:2016, Medical Devices - Symbols to be used with Medical Device Labels:
 |
This symbol indicates (and is located adjacent to) the date of product manufacture. The manufacture date is expressed in the form of a four-digit year, two-digit month, and (where appropriate) two-digit day. |
 |
This symbol indicates Use by and is located adjacent to the expiration date as cited in EN 28601. The Use by date is expressed in the form of a four-digit year, two-digit month, and (where appropriate) two-digit day. This symbol indicates that the device should not be used after the end of the month or day shown. |
Reference: ISO 15223-1:2016, Medical Devices - Symbols to be used with Medical Device Labels.
Q: What is the ECRI Institute and how can I become a member?
A: ECRI is an organization that performs independent medical device evaluations. This organization is designated an evidence-based practice center by the US Agency for Healthcare Research and Quality and is considered a federally certified patient-safety organization by the US Department of Health and Human Services.
The Army maintains an ECRI
Select-Plus subscription service. Anyone with a @mail.mil email address can request access. To become a member and receive access, send an account request to
tqmc@ecri.org. You must provide your name, military email address, and duty location. ECRI will respond by sending an email invitation for account setup. For additional questions call 610-825-6000 ext. 5891.
Upon creation of an ECRI account, access will be granted to the following services:
- Alerts Tracker: A web-based automated alerts management system that electronically distributes healthcare product safety alerts and recalls.
- Device & Supplier Profiles: A searchable database of medical product manufacturers, distributors, and the products they supply.
- Device Overviews & Specifications: A searchable database of technology overviews and product specifications for capital medical equipment.
- Pricing (Capital): A database of capital equipment and health information technology pricing used by hospitals to benchmark existing and proposed expenditures.
- Pricing (Supply & Implant): A database of medical/surgical supply and implant pricing used by hospitals to benchmark existing and proposed expenditures.
- TruVu: A visual, interactive complex decision making tool that engages stakeholders in an unbiased, transparent process that supports cost, quality, and outcome initiatives.
- Evaluations & Guidance: In-depth evaluations and comparative ratings on healthcare products. Expert guidance on hot technology topics.
- Healthcare Products Alerts: Safety alerts covering medical device problems, field corrections, and recalls along with ECRI Institute recommendations for follow up.
- Procurement Trends: Popular healthcare technology purchasing trends/market insights.
- Technology Trends: News articles on emerging medical technologies.
- Device & Supplier Downloadable Files: Downloadable files from medical product manufacturers and distributors and the products they supply.
- FDA Device Reports: Manufacturer/User Facility Device Experience (MAUDE) database.
- Financial Tools: analysis tools for key data related to medical device/healthcare technology selection decisions.
- Market Intelligence: Rapid access to market intelligence for healthcare decision makers.
- Technology Snapshot: Insight on top manufacturers, models, product specifications, price, and market trends.
- User Experience: User survey results on popular health technologies.
- Custom Analysis Dashboard: Personalized dashboard showing your recent activities, reports, and savings identified to date.
- Custom Technology Analyses: Expert advice on comparative effectiveness.
Reference: ECRI Website:
https://www.ecri.org/
Q: What is medical device lockout/tagout?
A: The control of hazardous energy is regulated under Occupational Safety and Health Administration (OSHA) Title 29 Code of Federal Regulation (CFR), Part 1910.147 (The Control of Hazardous Energy (Lockout/Tagout)). OSHA's lockout/tagout standard currently requires control of all energy sources (including energy stored within the medical device) during medical device servicing and maintenance through use of an Energy Isolating Device (EID). OSHA's definition of EIDs exclude the use of pushbuttons, selector switches, and other control-circuit type electrical-interruption devices:
- Lockout: Placement of a lockout device on an EID, in accordance with an established procedure ensuring that the EID and medical device being controlled can’t be operated until lockout-device removal.
- Lockout device: A device that uses a key or combination-type lock; blank flanges, or bolted slip blinds to hold an EID in a safe position preventing medical device energization.
- Tagout: Placement of a tagout device on an EID in accordance with an established procedure to indicate that the EID and medical device being controlled can’t be operated until tagout-device removal.
- Tagout device: A prominent warning device such as a tag securely fastened to an EID in accordance with an established procedure. This warning-tag ensures that the EID and medical device being controlled can’t be operated until tagout-device removal.
References:
- Title 29 CFR, Part 1910.147, The Control of Hazardous Energy (Lockout/Tagout)
- TB MED 750-2 - Operating Guide for MTOE Medical Equipment Maintenance, Section IV (Shop Safety), November 2006

Q: What Preventive Maintenance Checks and Services (PMCS) are required for the Impact (ZOLL) 754M Ventilator?
A: PMCS for the 754M Ventilator (LIN V99788, NSN 6515-01-648-5814) include cleaning, visual inspection of hoses, accessories, connections, and case; inspection and replacement of the anti-asphyxia leaf valve; air-inlet compressor filter check and replacement; battery care and recharging as well as performance checks and medical device calibration.
The following are operation and service manual sections and reference pages that discuss required maintenance tasks:
- Preventive Maintenance - Page 6-1 and 16-1.
- Operator Performance Check - Page 4-7.
- Cleaning - Page 6-1.
- Calibration - Page 6-1 and 14-1.
- Battery Care and Recharging - Page 7-1.
Reference: 754M Ventilator Operation and Service Manual, Rev 1.85R (06/07)
BACK TO TOP
Q: As a new maintainer what is one of the best references to find information on field maintenance operations?
A: There are several authoritative publication describing the intricacies of field maintenance operations, but as a new maintainer it would be recommended that a technician start with Department of the Army Pamphlet (DA Pam) 750-3, the Soldiers’ Guide for Field Maintenance Operations. This pamphlet takes the applicable maintenance regulations and provides a single go-to reference for and can be applied to any field maintenance operation.
References:
Q: What is the CBET certification and how can I earn it?
A: The CBET certification is a professional certification offered by the Association for the Advancement of Medical Instrumentation (AAMI) Credentials Institute specifically targeting the Biomedical Equipment Specialist (BES) field. Healthcare technology management professionals that desire a CBET certification are expected to have experience in a wide range of electromechanical devices, computers, networks, and software used in the delivery of healthcare. Any Soldier with a graduation certificate from the Medical Education and Training Campus Biomedical Equipment Specialist course qualifies to take the CBET exam.
Advantages for Army BES having earned the CBET include promotion points towards (E5 and E6) and higher rankings during the Senior Enlisted Promotion Boards (E7, E8, and E9) and Chief Warrant Officer Selection Boards.
The CBET exam its divided into 6 topic areas that include anatomy and physiology, public safety in the healthcare facility, fundamentals of electricity and electronics, healthcare technology and function, healthcare technology problem-solving, and healthcare information technology. Extensive preparation for this exam is highly encouraged, if not required, even for the most seasoned BES.
The AAMI offers a comprehensive interactive study course on their website at:
https://www.aami.org/training/healthcare-technology-management-(htm)
Access to free study materials can be found on the milSuite website at:
https://www.milsuite.mil/book/groups/dod-bmet-certification
A plethora of CBET study guides are also available which can easily be found by browsing the internet.
Once earned, the CBET certification must be maintained by collecting 30 continuing education units (CEUs) from six approved categories during a 3-year reporting period. The initial cost for taking the exam, subsequent renewal fees, and study materials may be paid for utilizing the Army Credentialing Assistance (CA) Program or the Federal Tuition Assistance (TA) Program. Contact your education center for guidance on utilizing these resources.
Other AAMI certifications related to the BES include Certified Radiology Equipment Specialist (CRES), Certified Laboratory Equipment Specialist (CLES) and Certified Healthcare Technology Manager (CHTM).
Reference: AAMI Website: https://www.aami.org
Q: How should the Portable Oxygen Generator System (POGS) feed-air compressor be installed and why is it important?
A: POGS feed-air compressor installation procedures are found in section 1.7 of the POGS installation manual (P/N P33C-MAN-INST-V1.2). Verify the power switch is in the off position before attaching the 208-volt alternating current three-phase power cable to the compressor. Follow all compressor motor-rotation instructions carefully. Avoid severe damage by ensuring current is properly phased to prevent the compressor motor from running in the reverse direction. Because phasing can differ between generators, repeat documented installation instructions anytime the POGS is relocated or the generator is changed. When energizing the feed-air compressor for the first time, momentarily apply power while simultaneously observing output-air directed from the right-side louvers of the compressor case. Strong air flow exiting the louvers indicate proper phasing. If air flow is not immediately observed, turn power off immediately. For improper current phasing, follow all safety precautions cited in POGS installation manual section 1.7.5, Correcting Reversed Feed-Air Compressor Rotation.
Reference: POGS Installation Manual, P/N P33C-MAN-INST-V1.2, On Site Gas Systems, Inc.,
https://a01.usamma.amedd.army.mil/mmip/Catalog/Item/015334481
Q: What is a maintenance significant medical device?
A: Army regulation (AR) 750-1 (Army Materiel Maintenance Policy) defines a maintenance significant medical device as an end item, assemblage, component, or system (intended for field issue to the Army) requiring recurring corrective maintenance services. Maintenance significant medical devices requiring maintenance while in storage generally have Line Item Numbers in the Army Maintenance Master Data File.
Reference: Army Regulation 750-1, Army Materiel Maintenance Policy
BACK TO TOP
Q: What is purpose of the 'Use by' date labeled on the outside of my battery kit? A:
A: The ‘Use by’ date is a supply-chain control specifying when batteries were last reconditioned to extend shelf life. This date typically reflects the battery with the shortest lifespan not necessarily everything in the kit so dates need to be properly analyzed.
Reference: US Army Medical Materiel Agency (USAMMA), Medical Maintenance Management Directorate (M3D)
Q: What are Scheduled Parts Replacements (SPRs) and how do I manage them?
A: SPRs fall into the Mission Essential Repair Parts (MERPs) category. These include non-demand supported, limited quantity, carefully selected (or Original Equipment Manufacturer (OEM) recommended) repair parts. MERPs are annually approved and signed by the unit commander for specific mission-critical medical devices authorizing on-hand use to meet an urgent service requirement. SPRs are performed at specific time or usage intervals and can often be identified in the technical manual 20 series, maintenance allocation chart, or in OEM service literature. SPR requisitioning is administered through your unit medical supply section, in accordance with internal standing operating procedures. While SPRs can be rapidly procured in garrison, always consider parts-item availability and the prospect of delays when procuring these items in a deployed environment. Advanced planning is a key factor in maintaining a properly functioning SPR program.
Reference: TB MED 750-2 (November 2006), Operating Guide for MTOE Medical Equipment Maintenance, Chapter 9, Paragraph 9-5 (Mission Essential Repair Parts) -
https://go.usa.gov/ x7QET
BACK TO TOP
- Determine operating conditions
- Assess system materials
- Evaluate ignition mechanisms (most applicable to BMETs)
- Determine kindling chain
- Analyze potential of loss of life, mission, or system
- Identify history of use
- Report
The emphasis of an OCA is to control of ignition mechanisms by minimizing heat sources and using materials that are not susceptible to igniting or sustaining fire.
BACK TO TOP
Q: What purpose do Prescribed Load Lists (PLLs) serve? What is shop stock?
A: PLLs are demand supported, non-demand supported, or new maintenance repair parts used for new end items. They are retained by units to support their daily maintenance program. To qualify as initial unit stockage, demand-supported maintenance repair parts must be ordered six (or more) times within an authorized control period. Army commands, Army service component commands, and direct reporting units have the ability to authorize 180- or 360-day control periods.
Shop stock is used for demand-supported repair parts and consumables that are stocked within an authorized support-level maintenance activity. This stock facilitates supported-unit maintenance requests or scheduled repairs. Shop stock is comparable to repair parts that are retained at the unit level for organizational maintenance. These parts are issued from a Supply Support Activity’s Authorized Stockage List (ASL) and can only be used for internal use.
Reference: AR 710-2, Inventory Management Supply Policy below the Wholesale Level; 2-21 and 2-23